A Danger to Future Generations

Source: CDC
Syphilis is a sexually transmitted infection (STI) that has been long nicknamed “The Great Pretender,” as its symptoms change over time and it can mimic many other diseases. Many thought “The Great Pretender” was nearly eliminated in the US as effective antibiotic treatment was widely available since the 1940s. Doctors, nurses and other clinical staff studied syphilis in textbooks, but were not seeing many cases in their practice. However, over the past decade, cases of syphilis began to re-emerge. According to the CDC, between 2014 and 2020 the national rate of total syphilis cases increased 175% (14.8 to 40.6 per 100,000). In 2020, the rate of reported new syphilis cases among American Indian and Alaska Native (AI/AN) persons was nearly four times the rate among non-Hispanic White persons (26.9 versus 6.9 cases per 100,000, respectively). The rate was particularly alarming for AI/AN females, at over seven times greater than the rate among non-Hispanic White females (21.3 to 2.9 per 100,000). It is important to note that these higher rates are not caused by race, ethnicity or heritage, but by social factors including difficulty accessing quality sexual health services, distrust of healthcare systems, fear of discrimination and negative feelings around testing and treatment for STIs.
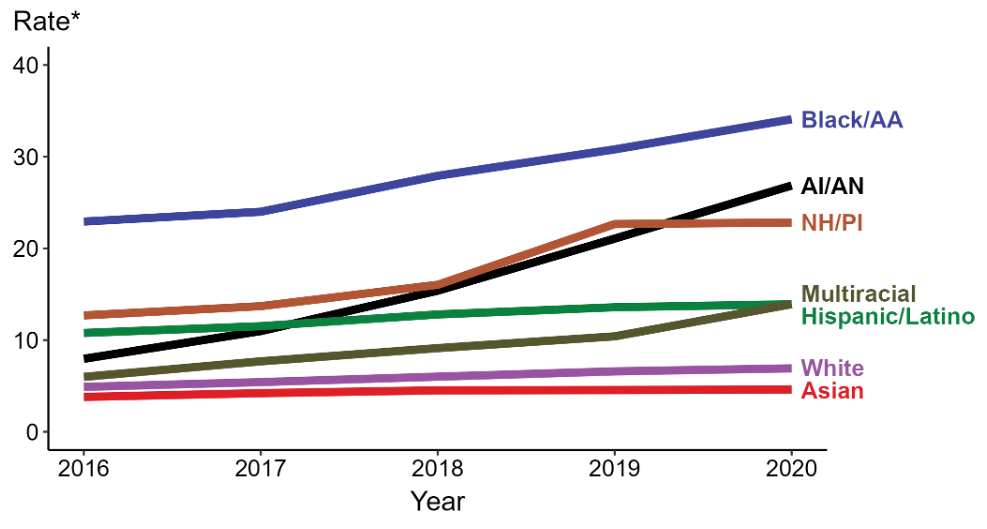
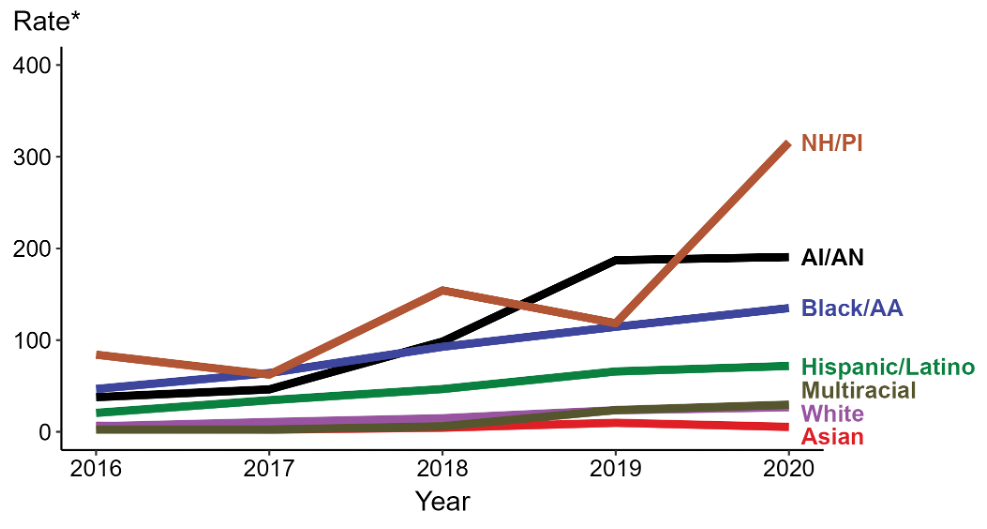
Syphilis can also be transmitted through the placenta from a mother to her unborn baby, referred to as congenital syphilis (CS). CS can be devastating, causing miscarriage, stillbirth, prematurity or infant death. CS can result in a wide range of clinical manifestations in surviving babies. Early findings can include rhinitis, hepatosplenomegaly, jaundice, osteochondritis, rash, ophthalmic disorders, lymphadenopathy, hematologic abnormalities and pseudoparalysis of extremities. Some newborns with CS are asymptomatic at birth but develop serious complications later in life without treatment. In children older than 2 years of age, CS may manifest as facial changes, perforation of the hard palate, abnormal tooth development, shortened maxilla, tibial thickening, ophthalmic disorders or deafness.When CS occurs, it is a marker of a significant amount of syphilis in the larger community. Communities in Indian Country are unfortunately experiencing this first-hand, and some are now facing high rates of syphilis and CS. Nationally, from 2016 to 2020, the rate of reported congenital syphilis increased over 400% among AI/AN babies (37.7 to 190.6 cases per 100,000 live births)
When CS occurs, it is a marker of a significant amount of syphilis in the larger community. Communities in Indian Country are unfortunately experiencing this first-hand, and some are now facing high rates of syphilis and CS. Nationally, from 2016 to 2020, the rate of reported congenital syphilis increased over 400% among AI/AN babies (37.7 to 190.6 cases per 100,000 live births).
Why is syphilis a problem?
While there is easy and effective antibiotic treatment available to cure syphilis, the diagnosis is often delayed. This contributes to ongoing disease transmission as well as serious health problems in some patients.
Syphilis can present in several stages. The first or primary stage of syphilis typically manifests as a small, painless sore on the genitals, called a chancre. It may not be noticed as it typically resolves even without treatment. Most patients who seek medical care for syphilis do so during the secondary stage several weeks later. During the secondary stage, symptoms may include a non-itchy rash on the palms and soles, sores in the mouth, vagina or anus, fever, swollen lymph nodes, sore throat, patchy hair loss, headaches, muscle aches, weight loss, or fatigue. Left untreated, later stage syphilis can cause hearing issues, paralysis, blindness, dementia and even death. These findings can present 10-30 years after the initial infection.
A pregnant woman can pass syphilis to her fetus during any stage of infection and at any trimester of pregnancy. However, the risk of transmission and serious disease is highest if the mother has been infected recently. Up to 40% of babies born to mothers with untreated syphilis who were infected within the four years prior to delivery are stillborn or die in infancy.
What can be done to address rising cases of syphilis?
Screening:
- More people need evaluation and screening for syphilis, including:
- Anyone with symptoms, or a partner with symptoms
- All pregnant women when they learn about their pregnancy, at 28 weeks and at their delivery
- Women who experience a stillbirth after 20 weeks of pregnancy
- People who are incarcerated
- People who use drugs
- People who exchange money or drugs for sex
- Newborns should not be discharged from the hospital unless the mother has been tested for syphilis at least once during pregnancy and at the time of delivery
- Consider using rapid testing for:
- People experiencing houselessness
- People accessing the Emergency Room or Urgent Care
- Local screening events
Know more about rates of syphilis in your community:
- Coordinate with tribal health departments, regional tribal epidemiology centers, local and state health departments to get information about new cases of syphilis – this is a notifiable condition
- Hire and train public health team members to assist with testing, contact tracing, case management and treatment of those with syphilis and their partners
Engage local medical providers:
- Ensure access to antibiotic treatment for people diagnosed with syphilis
- Make syphilis screening and sexual health visits routinely available
- Expand condom distribution campaigns
- Treatment should be offered to anyone who reports sexual exposure to someone with syphilis, even in the absence of signs or symptoms of infection
- While clinicians should test people exposed to syphilis, treatment should not be withheld while awaiting test results
To better protect tribal communities and future generations it is important to offer safe, supportive and judgement-free prenatal and sexual health care that readily offers these screening, treatment and prevention methods.
For more information please visit:
Works Cited:
The Facts – Syphilis (cdc.gov)
National Overview – Sexually Transmitted Disease Surveillance, 2020 (cdc.gov)
STD Facts – Syphilis (cdc.gov)
Increasing Congenital Syphilis in Oregon
Eitan Bornstein, MD | Epidemic Intelligence Service Officer (EISO)
Jessica Leston, MPH | Clinical Programs Director
Ashley Hoover, MPH | Communicable Disease Epidemiologist
Northwest Portland Area Indian Health Board