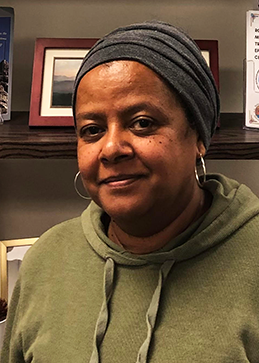
When you talk with Dr. Blythe Winchester, you can’t help but be drawn in by her stories. Her energy and passion for geriatric care is so engaging that she makes you feel that aging well isn’t just possible, it’s a human right. Blythe, a physician and member of the Eastern Band of Cherokee Indians, directs geriatrics at the Cherokee Indian Hospital in Cherokee, North Carolina. She has been a change maker at the individual level, through her Elder Care Specialty Clinic, and at the systems level, through her Dementia ECHO Program.
Every person has a story
“I realized that in geriatrics, what you care about most is a person’s story,” Blythe explained. “The most important thing is getting to know as much as you can about that person, their background, and their history. If you know a person’s story, those preferences and the things they have been through can be accounted for in their care plan so that they can age well.”
Starting an Elder Care Specialty Clinic
Understanding patients’ needs inspired Blythe to start an Elder Care Specialty Clinic at Cherokee Indian Hospital in 2013. To get the Clinic off the ground, Blythe spoke with administrators, sharing information about the care Elders deserve and the challenges many have in accessing that level of care.
Lucky for Blythe her insights were met with strong support. Once she had the go ahead, a dynamic team was formed using a patient-centered medical home model. As such, the Elder Care Specialty team included a nurse practitioner, RN case manager, certified medical assistant, and certified medical specialist. To address the needs of the whole person, the Clinic also included social workers, behavioral health providers, dietitians, and pharmacists.
Addressing polypharmacy and treating the whole person
One of the main goals of the Clinic is to ensure that the medications Elders are taking are necessary and appropriate. Blythe explained that “polypharmacy is often an issue. This occurs when an Elder is prescribed one medication, which causes side effects; then, another medication to counter those side effects, and the cycle continues.” When Elders enter the Clinic, one of the team’s first priorities is to target high-risk medication use that could be cause problematic side effects, such as memory issues, increased risk of falls, and retaining urine in the bladder.

Another goal of the clinic is to provide holistic care. So often, Blythe explained, primary care providers are taught to focus on a set of problems, rather than the whole person. “We ask questions about how well patients are getting around, how well they sleep, what their typical day is like, have they had any falls, how is their appetite and weight, and how is their mood. So each visit is more of a comprehensive look at that person, because doing so is how we help them stay at home as long as possible,” Blythe emphasized. Furthermore, screenings for abuse, food insecurity, and mold in the home are also routine. In addition, each visit involves discussing issues that might put a patient at high risk for dementia, such as unregulated blood sugar, lack of regular exercise, high blood pressure, and smoking. To help patients get wraparound services, social workers are embedded in the clinic and pharmacists provide medication education.
Providing a continuity of care
One of the strengths of the Elder Care Specialty Clinic is that it is embedded in the wider hospital system. When a patient from the Clinic needs a higher level of skilled nursing care, Blythe and her NP continue to see them at Cherokee’s skilled nursing care facility. Blythe and her team also have access to patients’ medical records if they go to the ER at Cherokee Indian Hospital. This not only helps patients receive a better continuity of services, it also helps Elders and their families feel supported and cared for.
From consultation to creating an ECHO program on dementia
Blythe has always envisioned the Clinic as having a dual role- treating patients and offering clinical consultation. One area that providers need frequent consultation on is screening, diagnosing, and treating dementia. When sharing information about this condition, Blythe would often hear, “Can’t I just clone you and bring you here?” This question sparked the idea to create an ECHO program focused on dementia.
To prepare, Blythe attended a training put on by Project ECHO at the University of New Mexico on how to create an ECHO. With this knowledge, support from Indian Country ECHO, help from a pharmacist at Cherokee Indian Hospital, and support from her hospital administration, Blythe hit the ground running. “I’ve never seen anything work that fast the whole time I’ve been in practice,” she reminisced. “Indian Country ECHO helped with sending emails, the technological aspects of running an ECHO, and advertising.

Using the ECHO model to improve Elder care
In alignment with treating the whole person, Blythe facilitates two types of ECHO sessions- one on dementia for clinicians and one on caregiver support for families. The dementia ECHO sessions for clinicians have a didactic portion, followed by a case presentation and discussion. The caregiver-focused ECHO sessions (part of the dementia ECHO program) similarly start with a didactic portion; however, to encourage peer learning, Blythe makes space for discussion. Blythe admitted that she was nervous that there would not be enough audience participation; however, once she opened the floor for questions, “both sessions just took off. Everyone had amazing discussion. It’s been wonderful so far. I can wait to see what comes.”
To enhance your ability to screen, treat and manage patients with dementia or offer quality caregiving support to a loved one with dementia, join the Dementia ECHO Program. Here you will participate in didactic and case presentations, receive recommendations from peers and specialists, and join a learning community committed to ensuring every person across Indian Country receives the high-quality healthcare they deserve.